-
Cosmedocs| Non Surgical
-
COSMESURG| Surgical
-
HARLEY STREET| Skin Care
FORMULATIONS -
| Skin Bar Clinic
 GLOW & GO
GLOW & GO
Impaired skin barrier and acid mantle function leading to sensitive skin issues
Human skin serves as an essential barrier against ultraviolet radiation, penetration of toxic compounds, surveillance of immune system and hydration of the body. The skin comprises of primary two layers – the epidermis and the dermis.The epidermis is where keratin, melanin and filaggrin are present. Langerhans cells are also present which regulate immune surveillance. Stratum corneum ( SC) is the outermost layer of the epidermis providing the barrier function of the skin. The SC is analogous to a ‘bricks and mortar’ structure in which keratin filled corneocytes act as ‘bricks’. Surrounding the bricks are lipid rich phase consisting of ceramide, fatty acid and cholesterol which makes up the ‘mortar’. Ceramide is a crucial component of the lipid bilayer in SC, and this helps to reduce transepidermal water loss. Proper hydration of SC is essential for optimum skin function. Natural moisturising factor ( NMF) production in SC is important in maintaining SC’s water binding capacity. Its main components are free amino acids, pyrrolidone carboxylic acid, lactate and filaggrin degradation products. Production of NMF is a multistep process within SC. NMF absorbs water from surroundings and retains it, increasing SC hydration. In situations of low humidity, production of NMF is increased to maintain hydration of SC. NMF causes pH of SC to be slightly acidic and protects it from over-degradation.
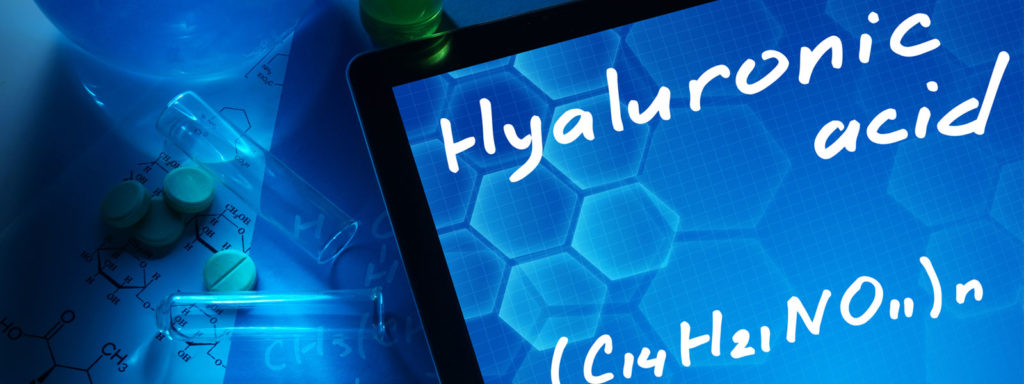
The dermis consists of collagen, elastin, glycosaminoglycans (GAG’s) which form the extracellular matrix. Dermis also contains blood vessels, nerves, lymphatics and sebaceous glands. Collagen is responsible for skin’s strength/structure and elastin provides elasticity of the skin. GAGs. GAGs consist of 4 groups: HSGAG and CSGAG, keratan sulphate types, hyaluronic acid. Hyaluronic acid is the most important component which helps to maintain dermis volume and skin turgor. GAGs also contribute to retain moisture and allows collagen to retain water. They also enable epidermis to be hydrated. Sebaceous gland produces acid mantle film which covers the skin. This slightly acidic layer acts a barrier to bacteria, viruses and other potential contaminants that might infiltrate the skin. Its pH ranges from 4.5-6.5.
Extrinsic and intrinsic factors can impair skin barrier. Examples of intrinsic factors are intrinsic ageing and many skin conditions (e.g. atopic dermatitis). We will go through how aging and atopic dermatitis cause changes in skin barrier in more depth. With age, multiple changes occur in the skin, both at the level of the epidermis and at dermis:
- Hyperkeratosis of SC
- Thinning of epidermis and dermis
- Reduced number of melanocytes and Langerhans cells.
- Collagen becomes less abundant, less soluble and thinner in the intrinsically aged skin. In photoaging, it is more soluble but thickened and fragmented.
- There is the greater production of defective elastin in the aged skin, and elastin degradation is slower with the accumulation of elastoic material.
- There is a more significant number of GAGs in the aged skin, but they are present on the elastoic material on the superficial dermis, hence are not able to bind to water well when distributed throughout the dermis.
- Ageing skin is less acidic than older skin due to the reduction in metabolic and enzymatic reactions.
Skin barrier impairment is thought to be the primary factor in the pathogenesis of atopic dermatitis leading to increased transepidermal water loss. Filaggrin mutations strongly predispose to development of atopic eczema. Filaggrin is primary source of several components of NMF. There is also change in intercellular lipid composition and arrangement in SC which reduce skin barrier in atopic eczema. There is less ceramide in atopic eczema leading to greater transepidermal water loss. Furthermore, in atopic dermatitis, there is an alteration in the immune system. It is a powerful, superantigen-driven vicious cycle involving T- helper type 2 dominated immune response, downregulation of antimicrobial peptides, S. aureus overgrowth and production of immunoactivation toxins with superantigenic properties. This interacts with an antigen –specific vicious circle involving IgE production and binding to high – affinity IgE receptors expressed on skin dendritic cells, followed by IgE- mediated, facilitated antigen presentation. An interaction of dysfunctional innate and adaptive immune responses in atopic dermatitis lesions may cause severe disease flares.
Common extrinsic factors that can affect skin barriers are UV rays, irritants, allergens, harsh cleansers, soaps and high heat/steam. Even water can affect skin barrier after a single wash. We will go through how cleansing can affect skin barrier in more detail.
Surfactants are active ingredients in cleaning products. Anionic surfactants are present in cleansers due to their high –foaming properties. However, they are alkaline and irritating to the skin.
Carboxylate –based soaps ( pH – 10) and their use transiently increases the alkalinity of skin post wash. PH of topically used products, even independent of surfactant has been shown to affect SC. Swelling of SC and increased rigidity of SC lipids is noted with topical products at pH 10. Note that most enzymatic process in skin function within relatively narrow pH window- hence, even brief increase in skin pH may disrupt biochemical processes of desquamation, lipid synthesis and NMF production. Also, surfactants in cleansers can directly bind and damage SC proteins as well as disrupt SC lipids. Furthermore, cleansing can result in leaching of NMF components from the skin, decreasing skin’s ability to hold moisture and contributing to post-wash dryness.
To maintain good skin barrier, we need to minimise exposure to extrinsic damage and have good effective skin care. Use of ultra – mild cleansers can help to reduce damage to both proteins and lipids in the skin during washing. For instance, directly esterified fatty isethionate ( DEFI ) cleaners protect SC lipids from extraction during cleansing due to the presence of skin identical fatty acids within surfactant system. Also, DEFI based cleansers can penetrate SC and replace lipid layer within SC as soon as they are lost.
Emollients are used to prevent trans-epidermal water loss. They do not provide moisture, but emollients can be used to deliver humectants ( e.g. glycerol) to hydrate SC. Formulations for emollients vary:
Ointments – oil based – more occlusive and more effective at reducing trans-epidermal water loss
Gels – provide water based delivery system whereby insoluble drug is mixed with gelling agents to aid absorption Creams and lotions are water based. Note water based products need preservatives to prevent bacterial contamination and growth. Hence, water based products may cause allergic contact dermatitis.
While emollients are useful to some degree, they only transiently ameliorate damage already done to the skin. However, some special topical agents can help to enhance skin barrier in targeted ways. Use of topical retinoic acid leads to compaction of stratum corneum, epidermal hyperplasia, correction of atypia, dispersion of melanin granules and increase in dermal collagen synthesis and angiogenesis. Peptides and proteins also have the ability to enhance collagen production. Niacinamide boots barrier function by increasing production of ceramide in SC.
References
- Wollenberg A et Al. Immunological and molecular targets of atopic dermatitis treatment. British Journal of dermatology ( 2014) 170, pp 7-11
- Janssens. M et Al. Lipid to protein ratio plays an important role in the skin barrier function in patients with atopic eczema. British Journal of dermatology ( 2014) 170, pp1248-1255
- Ananthapadamnabhan K.P et al. A global perspective on caring for healthy stratum corneum by mitigating the effects of daily cleansing: report from an expert dermatology symposium. British journal of dermatology ( 2013) 168, pp1-9
- Waller. J et al. Age and skin structure and function. Skin research and technology. 2006.12, pp145-154
- Cosmetic dermatology and non- invasive treatments. PG dip clinical dermatology Queen Mary university of London online learning environment 2015
- How to recognise and investigate skin disease. PG dip clinical dermatology Queen Mary university of London online learning environment 2015
Philip Gray
Related Posts
We use cookies to give you the most relevant experience, Cookie Policy.
See What Our Fellows Have Been Up to Recently
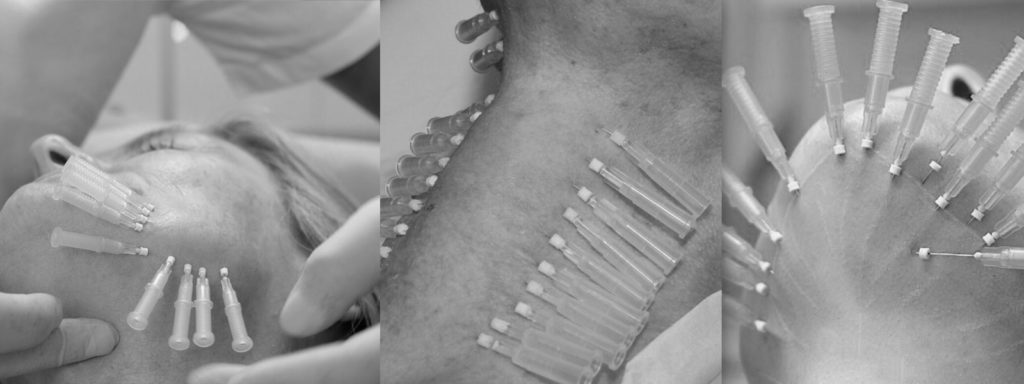
Historically, aspirating before administering certain injections, especially intramuscular ones, was standard practice. The main reason for aspiration was to avoid injecting medication directly into the bloodstream, which could cause adverse reactions or reduce the effectiveness of the medication.
However, the necessity and relevance of this practice have been debated in recent years. Some recent guidelines and studies suggest that aspiration may not be necessary for all types of injections. For example, it’s generally agreed that aspiration is not required for subcutaneous injections because there are fewer large blood vessels in the subcutaneous tissue that could be accidentally punctured. For intramuscular injections, the necessity of aspiration might depend on the injection site. For instance, aspiration is still recommended by some for injections in areas where large blood vessels are present, but it might be considered unnecessary for other sites.
The shift in practice is partly due to a better understanding of anatomy and the low risk of injecting into a blood vessel in certain areas, along with a desire to streamline the injection process and reduce patient discomfort. However, opinions and practices vary, with some healthcare professionals continuing to advocate for aspiration as a precautionary measure, while others view it as an unnecessary step for most injections.
#aestheticmedicine #dermalfiller #aceconference

Understanding depth, volume, and pressure can enhance a practitioner’s skill set, enabling them to provide more valuable services to their clients using their existing tools. #aestheticmedicine #dermalfillertraining #wrinklefree

Mastering hand stability isn’t magic, it’s a mix of experience & targeted learning 🎯 Our students get ahead with specialized techniques, paving the way for precise injections! 💉#SkillDevelopment #FutureHealthPros
.
.
.
.
.
#dermalfillertraining #aestheticmedicine #botoxtraining

Virtually any area can be reached using a cannula #fillertraining #aestheticmedicine #hsifellowprogram

“Unlock Your Aesthetic Potential with Harley Street Institute’s Fellowship! 🌟 Elevate your skills in aesthetic medicine through our intensive hands-on training in Botox and Dermal Fillers. Get ready to sculpt beauty, one injection at a time! 💉✨ Join us for a transformative learning journey that takes you beyond the classroom and into real-world expertise. Are you ready to master the art of enhancing natural beauty? 💫 #HarleyStreetFellowship #AestheticMedicineMastery #SculptingBeauty”

Link in bio
"Unlocking the Secrets of Masseter Botox: Empowering smiles, one injection at a time! 💉💪 Join me on an exciting journey as we delve into the world of Masseter Botox. Learn the art and science behind this transformative procedure, and discover how it can redefine facial aesthetics. Don`t miss out on this opportunity to enhance your skills and expand your practice. Let`s reshape faces and build confidence together!
Link in bio.
#MasseterBotoxCourse #FacialAesthetics #TransformativeProcedures #SmileEnhancement #ContinuingEducation
#aestheticmedicine

💭Have You Ever thought :
👉🏼What lies beneath the orbicularis oculi ?
👉🏼Why do I need to have the correct depth ?
👉🏼How to avoid an asymmetric smile, periorbital edema or a shelf like look at the lid/cheek junction ?
⚠️We all know that when treating crows feet, we are administering botox into the orbicularis oculi, and that there are complications but which and how?
‼️Too inferior or deep🟰 an asymmetric smile
(you’ve hit the zygomaticus minor muscle and major if you’re really too inferior!)
‼️Too medially 🟰 periorbital edema
(and you’re the periorbital region )
Located just underneath the skin, the orbicularis oculi has multiple origin and insertion points. A paired muscle, that overlies the periorbital region in a circular manner.
⚠️The wrong location, the wrong depth can result you injecting botox into a completely different muscle.

Welcome to the under eye region, an area of the face that can often show signs of aging such as wrinkles, hollows, and dark circles. Today, I want to share with you how fillers can be used to address these concerns by injecting them into different layers of the skin.
Using a needle, we can inject fillers into the dermis layer of the skin to improve the appearance of fine lines and wrinkles. This can help to smooth out the texture of the skin and create a more youthful and refreshed look. However, it’s important to note that injecting fillers into this layer requires specialized training and experience to ensure safe and effective results.
In addition to the dermis layer, fillers can also be injected into the bone to help address deeper hollows and shadows under the eyes. This technique requires a higher level of expertise as it involves precise placement of the filler to achieve the desired outcome.
Lastly, fillers can be injected into the fat compartment of the under eye region using a cannula. This method can help to add volume and smooth out any irregularities in the fat pads under the eyes. Again, specialized training and experience are crucial for safe and effective results.
Overall, the use of fillers in the under eye region can provide a non-surgical solution to address signs of aging and enhance the appearance of the face. However, it’s important to seek out a qualified and experienced provider who has received proper training in the use of fillers in this delicate area.
If you’re interested in learning more about how fillers can benefit you, please don’t hesitate to reach out and schedule a consultation. Let’s work together to help you achieve your aesthetic goals!
#cosmedocs #harleystreetinstitute
.
.
.
.
#lifestyleblogger
#selfcarematters #aestheticmedicine
#beautytips
#skincarecommunity
#antiagingtips
#makeuptutorials
#selfcarelove
#aestheticbeauty
#lifestyleinspo #lifestyleblogger
#selfcarematters #dermalfillertraining
#beautytips
#skincarecommunity
#antiagingtips
#makeuptutorials
#selfcarelove #dermalfillers
#aestheticbeauty
#lifestyleinspo
#antiagingsecrets
#harleystreet #drahmedhaq #oxforduniversity
#harleystreetinstitute

The mentalis muscle is a facial muscle located in the chin area. It originates from the mandible and extends downward to the skin of the chin. The primary function of the mentalis muscle is to control the movement and position of the lower lip and the skin of the chin. It plays an important role in activities such as speaking, smiling, and pouting.
In addition to its role in facial expression, the mentalis muscle also helps to maintain the position of the lower front teeth and the shape of the lower lip. Dysfunction or hyperactivity of the mentalis muscle can lead to the development of chin wrinkles, which are vertical lines that appear on the skin of the chin. Understanding the anatomy and function of the mentalis muscle is important for healthcare providers when performing aesthetic procedures in the chin area.
Online Course With Video Demo
www.harleystreetinstitute.com
#botoxtraining #mentalistreatment

#Repost @dranabilamzavala with many thanks 🙏 and best wishes for the future.
Esta semana tuve la oportunidad de estar en Londres en una de las mejores clínicas con los mejores equipos de Medicina Estética en el mundo, perfeccionado técnicas de Rinomodelación con el Dr.Ahmed Haq.
——
@drahmedhaq You are simply incredible, thanks for the hands on and all the new techniques you shared. @drahmedhaq @harleystreetinstitute @cosmedocs
.
.
.
#aestheticmedicine #dermalfillertraining #nosejob #medicaltraining #plab #harleystreet #10harleystreet #aesthetics

Huge Congratulations to Mariana, on completing her foundation course in Aesthetics Medicine with us here at Harley Street Institute. 🥇✨
This combined course covers the necessities required for daily clinic practise, whether starting out or refreshing skills. Our small group training (4:1) provide unparalleled mentorship at any of our training days.
#cosmetictraining #aesthetics #hsi #cosmetics #cosmedocs #harleystreetcourses #foundationcourse #london

Only courses with true mentorship. #botoxtraining #dermalfillertraining #aestheticmedicine #hsifellowprogram #harleystreetfellowship

Huge congratulations to @onemedicalclinic for completing her Fellowship in aesthetic Medicine with us at Harley Street Institute 💫💫✨ We are so proud of having you 🥰
#Repost
Dr Crystal:”When I completed medical school 13 years ago, one of my cherished mentors gave me advice that has stayed with me for life - “never stop learning; it makes the difference between being good and being great."
From my years of Ophthalmic-surgical training to becoming a student of Public Health to my experience as a legislator in Parliament to operating my own
Medical and Aesthetic Medical practice, the lessons learned have been varied and valuable. 🤓
On this occasion my commitment to lifelong learning led me to Harley Street, London. I didn’t just want to be a good injector, I needed to be a great one so I needed to go where the great injectors were. 💉
Every day for the last two months I was immersed in one-on-one intensive training with the aim of mastering my injectable skills and thanks to the incredible team of doctors and trainers at @cosmedocs
@harleystreetinstitute l am proud to say Mission Accomplished! “

Huge Congratulations to Dale Rae for completing the Certificate in Aesthetic Medicine training program. 💫💫
💉The 3-day Aesthetic Medicine Certificate is tailored towards new practitioners who are ready to kick-start their career in Aesthetic Medicine. It aims to provide an in-depth understanding of the Layers of the Skin and Biological Ageing Process. The package also includes our most popular Foundation Botulinum Toxin and Dermal Fillers course, including an introduction to using cannula.
💉It is an Intense 3-day course incorporating essentials basic and advanced botox and dermal filler procedures combined with popular skin treatments perfect for the beginner all-rounded aesthetic practitioner.
You will be provided direct mentorship by our various cosmetic practitioners who are experts in performing their respective aesthetic treatments.
💉Small group training under the direct supervision of our experienced aesthetic trainers. Master procedures to an advanced level. Learn theory, consultation methods and manage client expectations as well as complications.
🙌 DM for more details. #aesthetic #dermalfillers #detmalfillertraining

Aesthetic medicine is an art. It`s not enough to know facial anatomy or to be a good injector. The best aesthetic doctor has an artistic eye. Sometimes this is a skill that can be developed over years. Being able to assess a fa ce within seconds of walking into a room. Knowing exactly how injectables can be used for subtle and natural results.
The end result should not be obvious to an untrained eye.
It`s such a shame to see overfilled faces exaggerating proportions. When really, the main aims are to restore volume lost or correct natural imbalances.
#aestheticmedicine #dermalfillers #beauty
Repost @cosmedocs

Huge Congratulations to @erikatydermatology for completing her Fellowship in Aesthetic Medicine with us at the Harley Street Institute 💫💫💫
Our Aesthetic Fellowship is the pinnacle of training for those seriously interested in escalating their careers.
.
Our fellows are taken on board within clinic over 3 months with weekend workshops, 1-1 mentoring, treatment log book and clinical assistance.
.
Following on from this they have the opportunity to have Independent Fellow Clinics to improve their confidence with patient consultation and individual treatment planning.
.
We believe that this is the future of aesthetic traning to ensure that practitioners have captured all the essential skills for successful careers.
.
We have been extremely proud of our old fellows, many who have moved on to now work with some of the most prestigious clinics in London.
.
Next enrolment periods: TBC
.
To find out more information or to apply, please email your CV to [email protected]
.
#thefellowship #harleystreetinstitute #doctorsanddentists







Note: if you did not get the email, please check spam/junk folder