-
Cosmedocs| Non Surgical
-
COSMESURG| Surgical
-
HARLEY STREET| Skin Care
FORMULATIONS -
| Skin Bar Clinic
 GLOW & GO
GLOW & GO
Treatment of Danger facial areas with fillers
The use of latest generation of reticular purified hyaluronic acid for dermal filler treatment gives excellent results which last for 12-18 months in majority of the cases with minimal side effects.
The injections of hyaluronic acid should be followed by a use of the good aseptic technique. Usually, chlorhexidine is used for this purpose which is a good cleanser as well as a disinfectant. By using a good aseptic technique as well as the disposable and sterile materials, the risk of infections can be reduced to minimal. However, there is some possibility of subcutaneous bleeding suffusions which generally lasts for about 7-12 days. This can be accompanied by swelling or oedema of the treated area which usually subsides in 24-48 hours. There are few rare cases of erythema[1] that extended from the nasal tip and lasted for about 1 month.
Practically speaking, most of the complications of medical rhinoplasty occur due to accidental injections in regions of arterioles or venules with anterograde or retrograde embolization. The use of modern rhinoplasty materials particularly hyaluronic acid with medium reticulation does not cause edemas which sometimes occurs in and around the nasal region.
In the case of any accidental injection or any incorrect injection technique of hyaluronic acid into the blood vessels, the use of hyaluronidase is recommended by research studies[2][3]. The hyaluronidase should be injected as early as possible because its effectiveness of reducing the effects of hyaluronic acid decreases within four hours[4].
In injecting the nasal area, there can be instances of tissues distress due to injections into the intra-arterial region or due to extrinsic compression. Instances of blindness have also been reported due to injections of filler into the periocular area (mostly with fat injections but in few cases with hyaluronic acid and other types of resorbable fillers)[5][6][7]. It is certain that the nasal dorsal artery has retrogate communications with the central retinal artery as well as with internal carotid artery. That is why large boluses should be avoided while injecting in the danger areas including nasal ridge.
Guidelines for treating nasal ischemia from intra-arterial or para-arterial injections
Follow these latest guidelines and steps for injecting intra-arterial or para-arterial injections of hyaluronic acid for treating nasal ischemia[8][9][10].
- Ask the patients to sign an informed consent form in which it is written that the use of filler, in this case, is off-label and is not authorised in many European as well as extra-European
- Inform patient that the use of hyaluronidase can cause even strong allergic reactions.
- Don’t provide any treatment for common allergic reactions because allergy tests are not taken before administration, therefore, it is not known whether the treatment is preventing allergic reaction or stimulating it.
- Make a diluted solution of 150U of hyaluronidase with 1ml of 0.9% saline. There is no scientific research to support that using lidocaine without or with adrenalin is useful.
- Slowly inject minimal amounts from 0.05ml to 0.1 ml (7.5-15U).
- For superficial injection into the middle dermis, use 30G needle while for sub-dermis injections 27G needles can also be used.
- Nodule reduction is not instant but it becomes noticeable in 24-48 hours.
- The effectiveness of intra-artery injections is not supported by any scientific documentation. So if you decide to give these injections, it should be done in the shortest possible period as soon as ischemia and blanching are noticed in the nasal area where the patient may feel a dull burning sensation.
- In instance of noticeable blanching of the region, application of 5-10 mg nitroglycerine patch for 12 hours proves useful.
Injecting glabellar region
The glabellar region is a complicated area that is known for potential ischemia risks after filler or fat injections. The mechanism or emobilization in this region determine the appearance of complications which are not evidently identified but incorporate;
- A particular organisation and terminal division of the facial artery distant branches
- Product’s deep injection
- The sufficiently significant quantity of product being injected whose migration is likely to become more distal preventing contralateral supply.
In order to prevent such type of complication in the glabellar region, the injection technique used should be very superficial because the arterioles in this region are deeper located in the deep subcutaneous tissue or through the muscles[11],[12],[13]. It is necessary to avoid over-pressure during injection. In fact, using blunt cannula for injections in this region is a much safer option.
[1] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4248003/
[2] https://www.ncbi.nlm.nih.gov/pubmed/26964838
[3] Dr Maurizio Cavallini, Dr Riccardo Gazzola, Dr Marco Metalla, and Dr Luca Vaienti, ‘The Role of Hyaluronidase in the Treatment of Complications From Hyaluronic Acid Dermal Fillers’, Aesthetic Surgery Journal 33(8) (2013), 1167–1174
[4] Inglefield C, Collins F, Duckett M, Goldie K, Huss G, Paun S, Williams S, Expert consensus of Botulinum Toxin and Dermal Filler Treatment second edition (UK: Aesthetic Medical Expert Group, 2014)
[5] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3865975/
[6] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2686337/
[7] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4404720/
[8] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4298868/
[9] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4248003/
[10] Hwang Catherine J. Periorbital injectables: Understanding and avoiding complications. Journal of Cutaneous and Aesthetic Surgery. Year : 2016 | Volume: 9 | Issue Number: 2 | Page: 73-79
[11] Funt, D., & Pavicic, T. (2013). Dermal fillers in aesthetics: an overview of adverse events and treatment approaches. Clinical, Cosmetic and Investigational Dermatology, 6, 295–316. http://doi.org/10.2147/CCID.S50546
[12] Kim YK, Jung C, Woo SJ, Park KH. Cerebral Angiographic Findings of Cosmetic Facial Filler-related Ophthalmic and Retinal Artery Occlusion. J Korean Med Sci. 2015 Dec;30(12):1847-55. doi: 10.3346/jkms.2015.30.12.1847. Retrieved: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4689831/
[13] Peter, S. and Mennel, S. (2006), Retinal branch artery occlusion following injection of hyaluronic acid (Restylane). Clinical & Experimental Ophthalmology, 34: 363–364. doi:10.1111/j.1442-9071.2006.01224.x
Dr. A. Farhan Haq
Related Posts
We use cookies to give you the most relevant experience, Cookie Policy.

Botox & Dermal Filler Course
*excluding VAT

See What Our Fellows Have Been Up to Recently
Understanding depth, volume, and pressure can enhance a practitioner’s skill set, enabling them to provide more valuable services to their clients using their existing tools. #aestheticmedicine #dermalfillertraining #wrinklefree

Mastering hand stability isn’t magic, it’s a mix of experience & targeted learning 🎯 Our students get ahead with specialized techniques, paving the way for precise injections! 💉#SkillDevelopment #FutureHealthPros
.
.
.
.
.
#dermalfillertraining #aestheticmedicine #botoxtraining

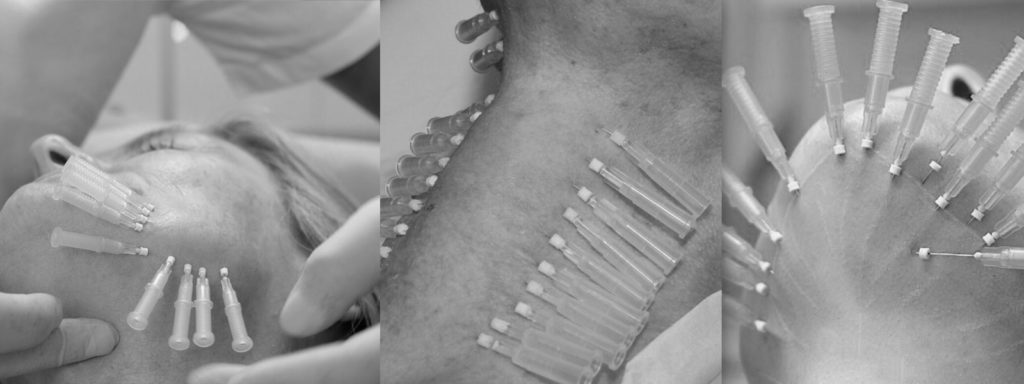
Virtually any area can be reached using a cannula #fillertraining #aestheticmedicine #hsifellowprogram

“Unlock Your Aesthetic Potential with Harley Street Institute’s Fellowship! 🌟 Elevate your skills in aesthetic medicine through our intensive hands-on training in Botox and Dermal Fillers. Get ready to sculpt beauty, one injection at a time! 💉✨ Join us for a transformative learning journey that takes you beyond the classroom and into real-world expertise. Are you ready to master the art of enhancing natural beauty? 💫 #HarleyStreetFellowship #AestheticMedicineMastery #SculptingBeauty”

Link in bio
"Unlocking the Secrets of Masseter Botox: Empowering smiles, one injection at a time! 💉💪 Join me on an exciting journey as we delve into the world of Masseter Botox. Learn the art and science behind this transformative procedure, and discover how it can redefine facial aesthetics. Don`t miss out on this opportunity to enhance your skills and expand your practice. Let`s reshape faces and build confidence together!
Link in bio.
#MasseterBotoxCourse #FacialAesthetics #TransformativeProcedures #SmileEnhancement #ContinuingEducation
#aestheticmedicine

💭Have You Ever thought :
👉🏼What lies beneath the orbicularis oculi ?
👉🏼Why do I need to have the correct depth ?
👉🏼How to avoid an asymmetric smile, periorbital edema or a shelf like look at the lid/cheek junction ?
⚠️We all know that when treating crows feet, we are administering botox into the orbicularis oculi, and that there are complications but which and how?
‼️Too inferior or deep🟰 an asymmetric smile
(you’ve hit the zygomaticus minor muscle and major if you’re really too inferior!)
‼️Too medially 🟰 periorbital edema
(and you’re the periorbital region )
Located just underneath the skin, the orbicularis oculi has multiple origin and insertion points. A paired muscle, that overlies the periorbital region in a circular manner.
⚠️The wrong location, the wrong depth can result you injecting botox into a completely different muscle.

Welcome to the under eye region, an area of the face that can often show signs of aging such as wrinkles, hollows, and dark circles. Today, I want to share with you how fillers can be used to address these concerns by injecting them into different layers of the skin.
Using a needle, we can inject fillers into the dermis layer of the skin to improve the appearance of fine lines and wrinkles. This can help to smooth out the texture of the skin and create a more youthful and refreshed look. However, it’s important to note that injecting fillers into this layer requires specialized training and experience to ensure safe and effective results.
In addition to the dermis layer, fillers can also be injected into the bone to help address deeper hollows and shadows under the eyes. This technique requires a higher level of expertise as it involves precise placement of the filler to achieve the desired outcome.
Lastly, fillers can be injected into the fat compartment of the under eye region using a cannula. This method can help to add volume and smooth out any irregularities in the fat pads under the eyes. Again, specialized training and experience are crucial for safe and effective results.
Overall, the use of fillers in the under eye region can provide a non-surgical solution to address signs of aging and enhance the appearance of the face. However, it’s important to seek out a qualified and experienced provider who has received proper training in the use of fillers in this delicate area.
If you’re interested in learning more about how fillers can benefit you, please don’t hesitate to reach out and schedule a consultation. Let’s work together to help you achieve your aesthetic goals!
#cosmedocs #harleystreetinstitute
.
.
.
.
#lifestyleblogger
#selfcarematters #aestheticmedicine
#beautytips
#skincarecommunity
#antiagingtips
#makeuptutorials
#selfcarelove
#aestheticbeauty
#lifestyleinspo #lifestyleblogger
#selfcarematters #dermalfillertraining
#beautytips
#skincarecommunity
#antiagingtips
#makeuptutorials
#selfcarelove #dermalfillers
#aestheticbeauty
#lifestyleinspo
#antiagingsecrets
#harleystreet #drahmedhaq #oxforduniversity
#harleystreetinstitute

The mentalis muscle is a facial muscle located in the chin area. It originates from the mandible and extends downward to the skin of the chin. The primary function of the mentalis muscle is to control the movement and position of the lower lip and the skin of the chin. It plays an important role in activities such as speaking, smiling, and pouting.
In addition to its role in facial expression, the mentalis muscle also helps to maintain the position of the lower front teeth and the shape of the lower lip. Dysfunction or hyperactivity of the mentalis muscle can lead to the development of chin wrinkles, which are vertical lines that appear on the skin of the chin. Understanding the anatomy and function of the mentalis muscle is important for healthcare providers when performing aesthetic procedures in the chin area.
Online Course With Video Demo
www.harleystreetinstitute.com
#botoxtraining #mentalistreatment

#Repost @dranabilamzavala with many thanks 🙏 and best wishes for the future.
Esta semana tuve la oportunidad de estar en Londres en una de las mejores clínicas con los mejores equipos de Medicina Estética en el mundo, perfeccionado técnicas de Rinomodelación con el Dr.Ahmed Haq.
——
@drahmedhaq You are simply incredible, thanks for the hands on and all the new techniques you shared. @drahmedhaq @harleystreetinstitute @cosmedocs
.
.
.
#aestheticmedicine #dermalfillertraining #nosejob #medicaltraining #plab #harleystreet #10harleystreet #aesthetics

Huge Congratulations to Mariana, on completing her foundation course in Aesthetics Medicine with us here at Harley Street Institute. 🥇✨
This combined course covers the necessities required for daily clinic practise, whether starting out or refreshing skills. Our small group training (4:1) provide unparalleled mentorship at any of our training days.
#cosmetictraining #aesthetics #hsi #cosmetics #cosmedocs #harleystreetcourses #foundationcourse #london

Only courses with true mentorship. #botoxtraining #dermalfillertraining #aestheticmedicine #hsifellowprogram #harleystreetfellowship

Huge congratulations to @onemedicalclinic for completing her Fellowship in aesthetic Medicine with us at Harley Street Institute 💫💫✨ We are so proud of having you 🥰
#Repost
Dr Crystal:”When I completed medical school 13 years ago, one of my cherished mentors gave me advice that has stayed with me for life - “never stop learning; it makes the difference between being good and being great."
From my years of Ophthalmic-surgical training to becoming a student of Public Health to my experience as a legislator in Parliament to operating my own
Medical and Aesthetic Medical practice, the lessons learned have been varied and valuable. 🤓
On this occasion my commitment to lifelong learning led me to Harley Street, London. I didn’t just want to be a good injector, I needed to be a great one so I needed to go where the great injectors were. 💉
Every day for the last two months I was immersed in one-on-one intensive training with the aim of mastering my injectable skills and thanks to the incredible team of doctors and trainers at @cosmedocs
@harleystreetinstitute l am proud to say Mission Accomplished! “

Huge Congratulations to Dale Rae for completing the Certificate in Aesthetic Medicine training program. 💫💫
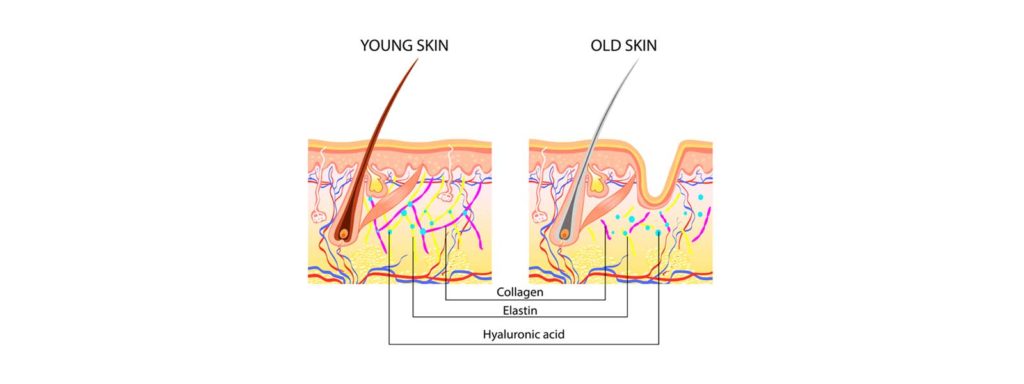
💉The 3-day Aesthetic Medicine Certificate is tailored towards new practitioners who are ready to kick-start their career in Aesthetic Medicine. It aims to provide an in-depth understanding of the Layers of the Skin and Biological Ageing Process. The package also includes our most popular Foundation Botulinum Toxin and Dermal Fillers course, including an introduction to using cannula.
💉It is an Intense 3-day course incorporating essentials basic and advanced botox and dermal filler procedures combined with popular skin treatments perfect for the beginner all-rounded aesthetic practitioner.
You will be provided direct mentorship by our various cosmetic practitioners who are experts in performing their respective aesthetic treatments.
💉Small group training under the direct supervision of our experienced aesthetic trainers. Master procedures to an advanced level. Learn theory, consultation methods and manage client expectations as well as complications.
🙌 DM for more details. #aesthetic #dermalfillers #detmalfillertraining

Aesthetic medicine is an art. It`s not enough to know facial anatomy or to be a good injector. The best aesthetic doctor has an artistic eye. Sometimes this is a skill that can be developed over years. Being able to assess a fa ce within seconds of walking into a room. Knowing exactly how injectables can be used for subtle and natural results.
The end result should not be obvious to an untrained eye.
It`s such a shame to see overfilled faces exaggerating proportions. When really, the main aims are to restore volume lost or correct natural imbalances.
#aestheticmedicine #dermalfillers #beauty
Repost @cosmedocs

Huge Congratulations to @erikatydermatology for completing her Fellowship in Aesthetic Medicine with us at the Harley Street Institute 💫💫💫
Our Aesthetic Fellowship is the pinnacle of training for those seriously interested in escalating their careers.
.
Our fellows are taken on board within clinic over 3 months with weekend workshops, 1-1 mentoring, treatment log book and clinical assistance.
.
Following on from this they have the opportunity to have Independent Fellow Clinics to improve their confidence with patient consultation and individual treatment planning.
.
We believe that this is the future of aesthetic traning to ensure that practitioners have captured all the essential skills for successful careers.
.
We have been extremely proud of our old fellows, many who have moved on to now work with some of the most prestigious clinics in London.
.
Next enrolment periods: TBC
.
To find out more information or to apply, please email your CV to [email protected]
.
#thefellowship #harleystreetinstitute #doctorsanddentists

KISS
As the years some procedures get unnecessarily more complicated without much added benefits. Risks / complications have increased: more inexperienced practitioners , inadequate techniques, increasing consumer demand for bolder augmentation.
#keepitsimplestupid






Note: if you did not get the email, please check spam/junk folder